Customer Stories
How Klear Care Runs a High Touch Psychiatry Practice Without Support Staff
15 mins saved
per patient
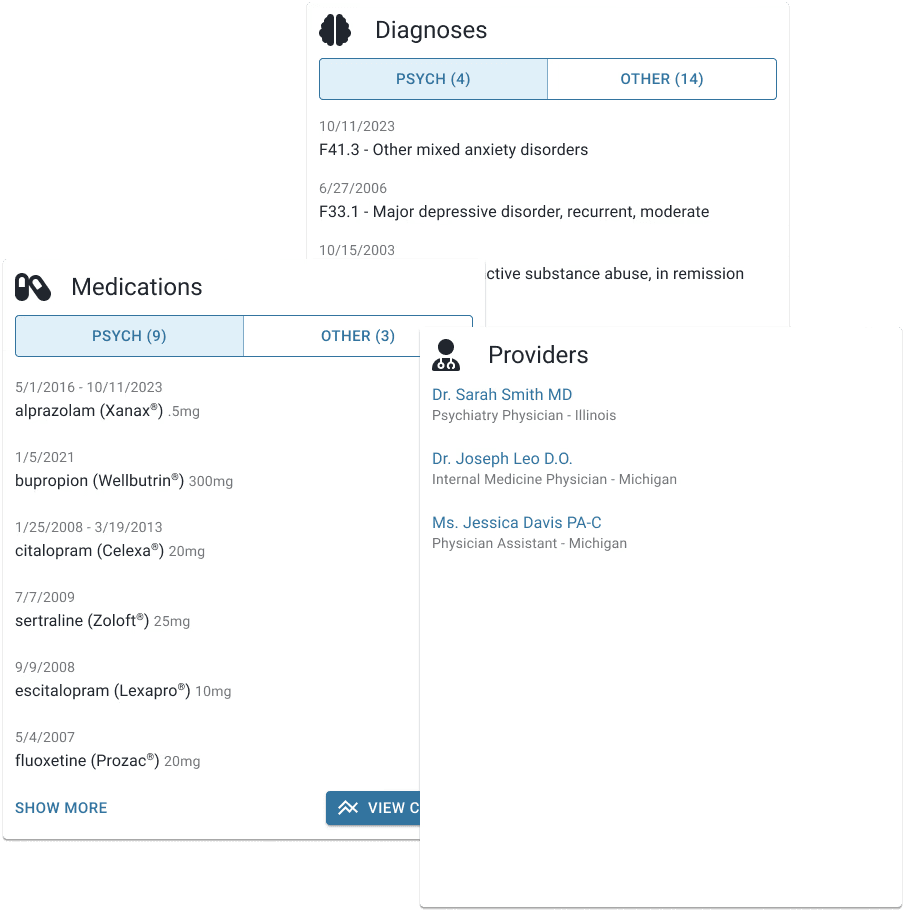
Psychiatric intake is now automated. Each patient’s medication history, labs, and background are ready before the first visit, giving Lindsay more time for meaningful clinical insight instead of data gathering.
More informed prescribing decisions
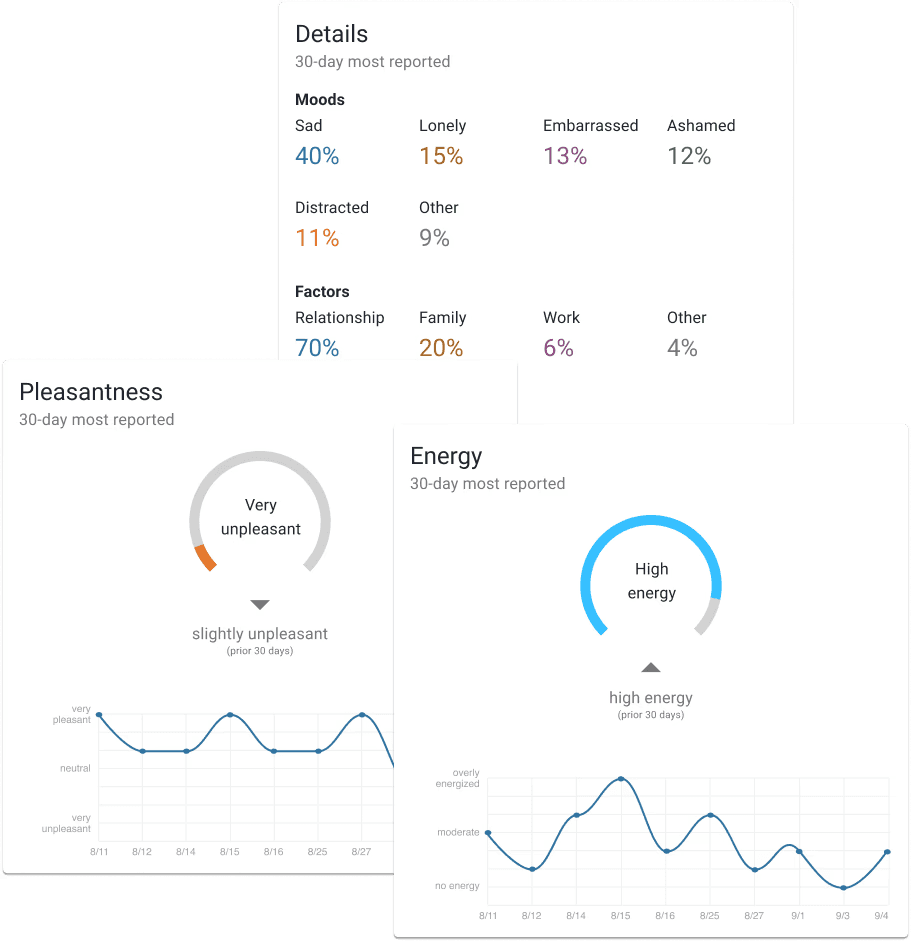
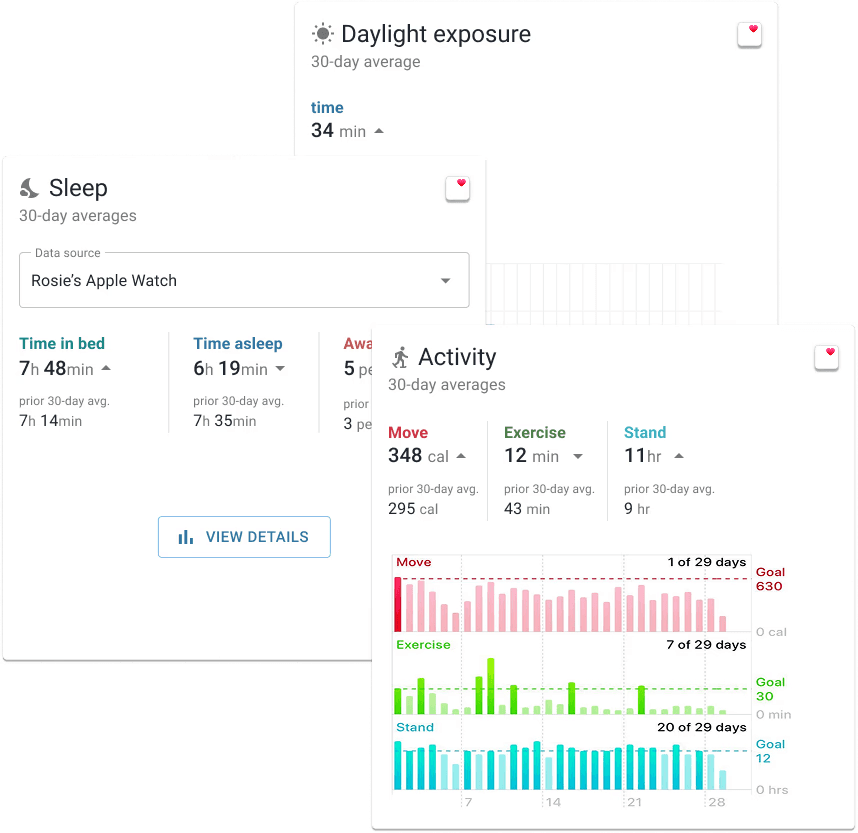
With behavioral and psychosocial factors like mood, sleep, lifestyle habits, and social context visible in one place, Lindsay has the clarity to make decisions that reflect the whole person.
A fully operational
solo practice
Headlamp automates intake and progress tracking, replacing multiple tools and the need for support staff. Klear Care runs smoothly with one system built for modern psychiatric care.
Meet the Experts Behind Headlamp Health
Dr. Lindsay Hill is the founder and CEO of Klear Care, a telehealth practice based in Phoenix, Arizona, focused on integrative and preventive psychiatry. She’s also the founder of PMHNP Bootcamp™, which has trained hundreds of Psychiatric Nurse Practitioners (PNPs), and the co-founder of The Psych NP Network, a national community for collaboration among PNPs.
Before launching Klear Care in 2022, Lindsay spent nearly eight years in community and insurance-based settings, including roles as Lead Psychiatric Nurse Practitioner at Crisis Preparation & Recovery and Phoenix Mental Health & Wellness. Those years shaped her perspective on how administrative burden and insurance-driven models limit time for thoughtful, patient-centered treatment.
Her goal with Klear Care was simple: build a practice that prioritized insight over volume. Many peers told her she’d need multiple systems, staff, and complex workflows to make it happen. She set out to prove there was another way.
“I got really burned out working at places where insurance started to dictate how I spent my time, what I documented, and even what I prescribed.”

Dr. Sarah Mitchell
Founder & Lead Psychiatrist at Klear Care
The Challenge
How Klear Care Uses Headlamp in Daily Practice
Building Rapport First, Tools Second
Lindsay introduces Headlamp at the second appointment, after establishing trust. By then, patients understand her clinical approach and are more receptive to tools that support their care.
“I got really burned out working at places where insurance started to dictate how I spent my time, what I documented, and even what I prescribed.”
Lindsay introduces Headlamp at the second appointment, after establishing trust. By then, patients understand her clinical approach and are more receptive to tools that support their care.
Making Data Meaningful
During appointments, Lindsay shares her screen while patients open the app on their phones. In 3 to 5 minutes, they review what the data reveals. The pie charts make invisible factors visible, whether it's grief, stress, or medical issues.
"I love the pie charts because I'm super visual. It's an easy way to see what's really going on for this person."
One patient's chart showed 80% of their distress came from grief after losing a pet. Without that visualization, Lindsay might have felt pressure to prescribe rather than simply hold space for a valid emotional response.
Connecting the Dots Over Time
Longitudinal data helps Lindsay and her patients identify patterns that might otherwise go unnoticed. When a patient developed daily migraines, the data showed a possible link to a medication started a year earlier.
“Sometimes you don’t put that together without that long-term view.”
The same insight applies to behavior change. Many patients only realize how much alcohol or screen time affects their sleep once they see it tracked over time.
“Knowledge doesn’t change behavior, but experience does. When patients can see their own data, it becomes personal.”
The Solution
Before and After: How Headlamp Transformed Lindsay’s Workflow
In community health, Lindsay often felt trapped by short appointments and incomplete information.
“It started to feel like symptom band-aiding, doing the best you can in a 20-minute med check.”
Private practice gave her more control, but she still needed a way to see the full picture without drowning in paperwork. Headlamp changed how she structures care from intake to follow-up.
Initial Psychiatric Evaluations
Before Headlamp
First 15 minutes spent collecting medication history, medical conditions, and provider details
Manual record requests from multiple providers
Patients struggled to remember their full medical background
After Headlamp
Lindsay starts every evaluation with complete context and saves about 15 minutes per patient
Headlamp automatically organizes data in the provider dashboard
Patients complete their medication history, conditions, and provider info before the visit
Follow-up Appointments
Before Headlamp
Depended on patient recall for sleep, alcohol use, or lifestyle changes
Hard to connect behavioral patterns to symptoms
Pressure to adjust medications quickly
After Headlamp
Patients spend two to five minutes tracking mood, sleep, and daily habits
Lindsay reviews longitudinal data before each appointment
Together, they look at trends that guide treatment decisions
Administrative Tasks
Before Headlamp
Writing prior authorization letters for TMS and newer medications
Filling out paperwork to prove medication trials
Assigning staff to gather documentation
After Headlamp
Medication trials and symptom trends are available instantly
Screenshots replace multi-page forms for faster approvals
No virtual assistant or additional staff needed
The Impact
The Impact: A Leaner, Efficient Practice
Time saved from intake and documentation now goes directly into patient care. Lindsay saves about 15 minutes per patient, adding up to hours each week that she reinvests into her practice and professional community.
“I don’t have a virtual assistant, which surprises people. But I don’t need one. The right automation makes it possible to run my practice efficiently on my own.”
Headlamp reinforces Klear Care’s philosophy: slowing down medication decisions, validating patient experiences, and grounding care in real-world data. Patients are more engaged and more accountable, spending just a few minutes between sessions tracking habits that improve outcomes.
“Headlamp helps me and my patients look at the whole picture. It keeps us focused on progress, not just prescriptions.”
Lindsay’s ideal patients are those who want to take an active role in their care and aren’t looking for a quick fix. Many come through therapy referrals after realizing they’ve done the work but still need clinical support. Headlamp helps them stay connected between visits and gives Lindsay the clarity to guide progress over time.